Good Medicine, Bad Behavior: Drug Diversion in America
Explore the Exhibit
Pain Management
- Introduction
- History of Pain
- Prescribing Today

Prescription medicines.
What is Pain Management?
Pain management generally benefits from a multidisciplinary approach that includes pharmacologic measures (analgesics such as narcotics, and pain modifiers such as antidepressants or anticonvulsants), non-pharmacologic measures (such as interventional procedures, physical therapy and physical exercise, application of ice and/or heat), and psychological measures (such as biofeedback and cognitive therapy).
Chronic Pain vs. Acute Pain
Acute pain, such as occurs with trauma, often has a reversible cause and may require only transient measures and correction of the underlying problem. Chronic pain is different. Chronic pain persists. Pain signals keep firing in the nervous system for weeks, months or even years. There may have been an initial mishap—sprained back, serious infection, or there may be an ongoing cause of pain—arthritis, cancer, ear infection. Some people suffer chronic pain in the absence of any past injury or evidence of body damage. Many chronic pain conditions affect older adults. Common chronic pain complaints include headache, low back pain, cancer pain, arthritis pain, neurogenic pain (pain resulting from damage to the peripheral nerves or to the central nervous system itself), psychogenic pain (pain not due to past disease or injury or any visible sign of damage inside or outside the nervous system). American Pain Foundation
Incidents of Pain
- More than one-quarter of Americans (26%) age 20 years and over—or, an estimated 76.5 million Americans—report that they have had a problem with pain of any sort that persisted for more than 24 hours in duration.
- Adults age 45-64 years were the most likely to report pain lasting more than 24 hours (30%). Twenty-five percent (25%) of young adults age 20-44 reported pain, and adults age 65 and over were the least likely to report pain (21%).
- More women (27.1%) than men (24.4%) reported that they were in pain.
- Non-Hispanic white adults reported pain more often than adults of other races and ethnicities (27.8% vs. 22.1% Black or 15.3% Hispanic).
- Adults living in families with income less than twice the poverty level reported pain more often than higher income adult
National Center for Health Statistics
Pain in Every Day Life
- The annual cost of chronic pain in the United States, including healthcare expenses, lost income, and lost productivity, is estimated to be $100 billion. NIH
- More than half of all hospitalized patients experienced pain in the last days of their lives and although therapies are present to alleviate most pain for those dying of cancer, research shows that 50-75% of patients die in moderate to severe pain. SUPPORT
- An estimated 20% of American adults (42 million people) report that pain or physical discomfort disrupts their sleep a few nights a week or more. National Sleep Foundation
References
National Institutes of Health. NIH Guide: New Directions in Pain Research I. September 4, 1998. Available from http://grants.nih.gov/grants/guide/pa-files/PA-98-102.html
SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA.1995; 274:1591-1598
Weiss SC, Emanuel LL, Fairclough DL, Emanuel EJ. Understanding the experience of pain in terminally ill patients. Lancet. 2001; 357:1311-1315
National Sleep Foundation. Sleep in America poll. 2000. Available from: http://www.sleepfoundation.org
A History of Pain Relief
In ancient China and India and pre-Columbian America, natural anesthetics were used to ease some types of pain, including that associated with surgical procedures. In the first century, the Greek physician and naturalist Dioscorides suggested that the root of the mandragora plant steeped in wine be given to patients before flesh or limbs were cut. It was in 1842 that the first doctor administered ether for surgery
Timeline for Pain Management
4000 BC -
Opium poppy seedpods found in Swiss lake dwellings may have been used for dulling the senses.
1500 BC -
Caravans from ancient China bring natural anesthetics and soporifics to the West.
100 AD -
Roman naturalist Pliny reports use of the “potion of the condemned” to reduce the pain of crucifixion.
1020 AD -
Avicenna of Persia teaches that opium is “the most powerful of stupefacients.”
1790 -
Philip Syng Physick, the father of American surgery, occasionally bleeds patients to near collapse to decrease pain sensitivity. 1803
Pharmacist Friedrich Serturner isolates morphine from opium.
1830 -
Napoleon's chief surgeon, Dominique-Jean Larrey, espouses carbon dioxide anesthesia to induce “suspended animation.”
1850 -
James Simpson experiments with chloroform and convinces Queen Victoria to use it during childbirth.
1850s -
The hypodermic syringe is perfected and introduced into medical practice.
1884 -
Sigmund Freud believes cocaine can combat pain and encourages a colleague to use it for eye surgery.
1895 -
Heroin is synthesized from morphine giving a more potent but more addicting pain reliever.
1898 -
Aspirin is synthesized and is the first relatively safe non-addicting pain reliever.
1955 -
Acetaminophen is introduced and becomes the number one non-prescription pain reliever.
1990 -
Pain relief on demand becomes more common as quality-of-life issues supersede fear of addiction.
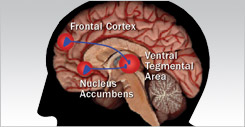
2000-Future - Better understanding of brain and nerve interactions leads to techniques for preventing pain before the brain can recognize it.
The Reality
Opioid painkillers now cause more drug overdose deaths than cocaine and heroin, combined. CDC
Prescriptions For Pain
The top prescription drug sold in the United States in 2005 and 2006 was hydrocodone with acetaminophen, with more than 211 million prescriptions written. The United States used 99% of the global supply of hydrocodone in that time. IMS Health
Tracking An Increase in Abuse
The recent increase in the extent of prescription drug abuse in this country is likely the result of a confluence of factors, such as: Significant increases in the number of prescriptions; significant increases in drug availability; aggressive marketing by the pharmaceutical industry; the proliferation of illegal Internet pharmacies that dispense these medications without proper prescriptions and surveillance; and a greater social acceptability for medicating a growing number of conditions. NIDA
The Power and Danger of the Internet
It is becoming increasingly easy for persons of any age to obtain controlled substances illegally by means of the Internet. Numerous Web sites based in the United States and abroad sell controlled substances to anyone willing and able to provide a credit card number. Some of these Web sites do not require a prescription. Others will provide the buyer with an illegitimate prescription simply by having the buyer fill out an online questionnaire without seeing a physician. DEA
The Standard for Prescribing Controlled Substances
Prescriptions for controlled substances must be issued for a legitimate medical purpose by a registered physician acting within the usual course of professional practice. This should in no way interfere with the legitimate practice of medicine or cause any physician to be reluctant to provide legitimate pain treatment. DEA
Limits of the Law
While the Controlled Substances Act (CSA) is one component of the overall regulation of the practice of medicine in the United States, the CSA does not regulate the practice of medicine. The CSA regulates only the segment of medical practice involving the use of controlled substances, and DEA is correspondingly responsible for ensuring that controlled substances are used in compliance with Federal law. DEA
A History of Regulation
For more than 90 years (starting with the Harrison Narcotic Act of 1914, which was superseded by the CSA in 1970) Federal law has placed certain restrictions on the medical use of federally controlled substances while, at the same time, the States have regulated the practice of medicine generally. DEA
Regulation is State By State
Beginning in the 1930s and through to the present, States have adopted uniform controlled substance laws that were designed to promote standards that are consistent from State to State and in harmony with Federal law. DEA
State Medical Boards
State laws and State licensing bodies (such as medical licensing boards) collectively regulate the practice of medicine. Each State also has its own laws (administered by State agencies) requiring that a prescription for a controlled substance be issued only for a legitimate medical purpose by State-licensed practitioners acting in the usual course of professional practice. DEA
Enforcement by Federal and State Officials
A practitioner who dispenses controlled substances for other than a legitimate medical purpose, or outside the usual course of professional practice, is subject to legal liability under both State and Federal law. DEA
How to Determine Over-Prescribing
There are no specific guidelines concerning what is required to support a conclusion that an accused doctor acted outside the usual course of professional practice when prescribing medicines for pain. Rather, the courts must engage in a case- by-case analysis of evidence to determine whether a reasonable inference of guilt may be drawn from specific facts. DEA
Cases Against Doctors
Cases in which physicians have been found to have dispensed controlled substances improperly under Federal law generally involve facts where the physician's conduct is not merely of questionable legality, but instead is a glaring example of illegal activity. DEA
Striking A Balance
The challenge is to eliminate or significantly curtail diversion and abuse of controlled prescription drugs while assuring proper treatment of patients who can be helped by these medications.
Establishing Standards for Managing
Pain
There is a lack of consensus among physicians as to all the circumstances that warrant the use of opioids to treat pain. It may be impossible to provide an exhaustive and foolproof list of "dos and don'ts'' when it comes to prescribing controlled substances for pain or any other medical purpose. The courts have recognized that there are no definitive criteria laying out precisely what is legally permissible, as each patient's medical situation is unique and must be evaluated based on the entirety of the circumstances. DEA
How Much Is Too Much?
What constitutes “an inordinately large quantity of controlled substances” can vary greatly from patient to patient. A particular quantity of a powerful schedule II opioid might be blatantly excessive for the treatment of a particular patient's mild temporary pain, yet insufficient to treat the severe unremitting pain of a cancer patient. DEA
How Many Doctors Are Breaking the Law?
The overwhelming majority of American physicians who prescribe controlled substances do so for legitimate medical purposes. In any given year, including 2005, fewer than one out of every 10,000 physicians in the United States (less than 0.01 percent) lose their controlled substance registrations based on a DEA investigation of improper prescribing. Even in the rare cases where a physician loses his/her DEA registration for improper prescribing, it is often State officials—not DEA—who initiate the investigations. DEA
Educating the Medical Community
The responsibility for educating and training physicians so that they make sound medical decisions in treating pain (or any other ailment) lies primarily with medical schools, post-graduate training facilities, State accrediting bodies, and other organizations with medical expertise. DEA
Looking to the Future of Pain Management
With an aging population and the development of new and more sophisticated chemical substances to manage and treat pain, this issue will not be going away any time soon.
Introduction

Explore the rise of patent medicine industry from the late 1800s through to modern day prescription drugs.
Learn More
Learn More
History of Prescription Drugs

Explore the revolution in therapeutics during the past 120 years. Medicines have been discovered to cure disease and to relieve pain.
Learn More
Learn More
The Science of Drugs
Explore the many substances found to have wonderful healing and pain-relieving properties, but also many that could cause harm if used incorrectly.
Learn More
Learn More
The Controlled Distribution System

Explore the various laws and regulations have been passed by the federal and state governments to regulate and control the manufacture, distribution and dispensing of medicines.
Learn More
Learn More
Prescription Fraud

Explore the laws put in place in response to growing abuse and addiction problems with controlled substances.
Learn More
Learn More
Diversion of Chemicals

Explores the clandestine production of drugs, which is dependent on the availability of chemicals necessary to produce the illicit drug activity.
Learn More
Learn More
Pain Management

Explores the critical balance between promoting pain relief and preventing the diversion and abuse of powerful prescription drugs.
Learn More
Learn More
Lost Talent
Discovery Corner